
With regard to personality disorders, a common comorbid condition of DPD patients, a recent study found no differences between n = 24 patients with borderline-personality disorder and healthy controls concerning their performance on measures of interoceptive accuracy. In summary, there is some evidence for an association of trait anxiety or anxiety disorders with increased interoceptive accuracy as measured by heartbeat detection tasks. No differences were found between panic disorder and other anxiety disorders.
With regard to anxiety disorders, a pooled analysis of heartbeat perception studies suggested that accurate heart beat perception is more prevalent among panic disorder patients than in healthy controls, depressed patients, or patients with palpitations or individuals with occasional panic attacks. In a study investigating a small sample of 18 patients with major depression, patients performed equally well compared to healthy controls on the heartbeat detection task and better than a less depressed community sample with moderate depression. However, there was an interaction with the level of anxiety in this non-clinical sample: In highly anxious individuals depression was negatively correlated with interoceptive accuracy, while there was a positive correlation for persons low in anxiety. A recent study of a large non-clinical sample showed heartbeat perception to be positively correlated with anxiety and negatively with depression. For example, comorbid depression and anxiety may have differential effects on interoceptive accuracy. It is surprising, therefore, that there are currently no published reports on interoception in DPD patients using experimental interoception tasks.Īs anxiety disorders and depression are frequent comorbid conditions in patients with DPD, ,, these comorbidities need to be taken into account when investigating interoceptive accuracy of DPD patients. Therefore, given the profound disruption of self-awareness, mainly characterized by feelings of disembodiment and emotional numbing, together with the neurobiological findings of an inhibition of insular activity, DPD may be considered as a specific disorder of embodiment and thus specific impairments of interoception as measured by heart beat detection tasks, , –.
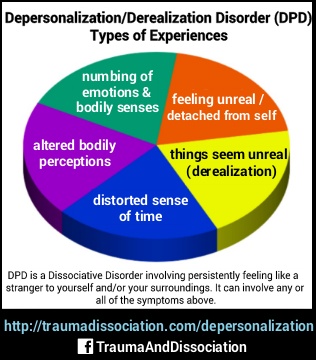
#Depersonalization derealization disorder series
It is assumed that self-awareness is continually regenerated in a series of bodily signals which blend together to give rise to a continuous “stream of consciousness”. Interoception and emotional feelings are considered as the fundament of the embodied self. Recently it has been shown that self-focused attention, which is considered as crucial factor for the maintenance of depersonalization, –, correlated inversely with the sensitivity toward one's cardiac signals. Another cause of impaired interoception in DPD patients may be their increased self-focused attention. (2000) found aberrant glucose metabolism in temporal, parietal, and occipital areas, and functional abnormalities of the secondary and cross-modal sensory cortex as well as areas responsible for an integrated body schema. Further biological evidence for the profound subjective distortions of body awareness in DPD patients comes from a study using positron emission tomography to assess brain glucose metabolism of patients with DPD as compared to healthy controls: Simeon et al. Substantial studies and publications suggest that the intensity of emotional experiences, which is specifically attenuated in DPD patients, , depends on interoceptive awareness, –. Further, it has been shown that interoception and emotional processing are closely related. There is ample of evidence that the degree of interoceptive awareness can be conceptualized as a trait-like sensitivity toward one's cardiac or visceral signals. Its activity correlates strongly with interoceptive awareness as measured by heart beat detection tasks. In particular the insular cortex is responsible for the representation of visceral sensations accessible to awareness. Both structures are crucial for interoception. Results from neuroimaging studies, though rare, show reduced activation of the insular and the anterior cingulate cortex in response to aversive affective stimuli in DPD patients as compared to healthy controls or patients with obsessive compulsive disorder.

Narratives of disembodiment as described by the items of the Anomalous Body Experiences subscale of the Cambridge Depersonalization Scale


 0 kommentar(er)
0 kommentar(er)
